Can Thyroid Hormone Levels Affect Breastfeeding?
Having thyroid issues is not ideal for any of us during any period in our lives, but it is especially not welcomed during periods in which people are pregnant or breastfeeding.
In the following article, we will explore the potential dangers that come with the most common thyroid issues and their impact on the ability to breastfeed your child.
Can you breastfeed if you are dealing with thyroid issues?
Through the process of breastfeeding, babies are offered nutrient and antibody-rich milk that they need in order to develop and grow properly.
Breastfeeding your baby can protect it against multiple health issues such as development problems, diabetes, allergies, asthma, etc. Breastfeeding is beneficial for nursing mothers as well, as it reduces the risk of ovarian and breast cancer.[i]
Unfortunately, thyroid problems are compromise the breastfeeding process.
As you may know, prolactin is the hormone that is produced during pregnancy and the breastfeeding due to its role to enable the production of milk within mammals. The pituitary gland is responsible for the production and secretion of prolactin into the bloodstream.
The normal prolactin levels within breastfeeding women are considered to be around 10-209 ng/mL. Past research has shown that there is a close link between thyroid hormones, thyroid-releasing hormone (TRH) and prolactin levels.
The TRH stimulates the secretion of prolactin, so issues related to the prolactin secretion are expected to develop due to any thyroid issues that the nursing mother experiences due to any reason.[ii]
Thyroid issues have been reported to occur before and during pregnancy, in the postpartum period, and later during the lifetime. It is essential to treat these issues as soon as possible, as thyroid glands have a big impact on our overall health.
Breastfeeding while dealing with an untreated thyroid issue of any kind can be quite challenging.
Breastfeeding while struggling with thyroid issues
In the following section, we will explore some of the most common thyroid issues that past nursing mothers have reported to experience.
You will learn their symptoms and how to recognize them while in their most early stages, but also, learn how these specific issues are affecting your ability to breastfeed your little one.
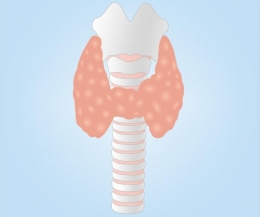
Hypothyroidism
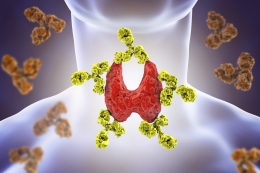
Hypothyroidism, also known as underactive thyroid, is a common thyroid issue. In most cases, it is caused by Hashimoto’s thyroiditis, an autoimmune disease in which the patient’s immune system attacks the thyroid gland, causing inflammation to develop.
Symptoms of hypothyroidism include weight gain, fatigue, constipation, depression, dry skin, hair loss, and many more. Hypothyroidism is most commonly treated with the use of synthetic thyroxine known as levothyroxine.
It is of vital importance for hypothyroidism symptoms to be recognized in time and treated properly.
Hypothyroidism is linked to numerous issues that can develop before, during, and after pregnancy.
Low thyroid levels and elevated thyroid-stimulated hormone (TSH) levels cause high prolactin levels.
There is also the issue of TSH being secreted into the breastmilk, which is suggested to cause thyroid disorder conditions to develop in the nursing infant.
But hypothyroidism also causes weight gain, which during pregnancy increases the risk of gestational diabetes, miscarriage, sleep apnea, cardiac dysfunction, etc.[iii]
But the most important issue of them all is the reduced milk supply that a breastfeeding mother with hypothyroidism issues faces during this time. Without an adequate milk supply, your baby will fail to gain weight in a healthy matter, and with that, fail to develop and grow as it is supposed to.
Most treatment protocols study, suggest that taking levothyroxine to increase the thyroid hormone levels, reflects positively on milk production, as nursing mothers no longer experience breastfeeding issues. [iv]
In addition, Hypothyroidism, as mentioned earlier, commonly causes depression to develop. This means that hypothyroidism directly increases the risk of postpartum depression, which comes with major risks on its own.[v]
Hyperthyroidism
Contrary to hypothyroidism, hyperthyroidism represents a condition of an overactive thyroid gland, where the thyroid hormones are being produced and secreted in excessive amounts.
Grave’s disease is the most common cause of hyperthyroidism.
The common symptoms of hyperthyroidism include swelling of the thyroid gland or an enlarged thyroid gland, fatigue, diarrhea, muscle weakness, increased appetite, weight loss, mood swings, and oversensitivity to heat among many others. Hyperthyroidism is efficiently treated with the use of thyroid drugs, radioactive iodine, and surgery.
Hyperthyroidism is also recommended to be treated as soon as possible, as a way to enhance the quality of the breastfeeding experience.
Hyperthyroidism, due to Grave’s disease, is often mistaken for the hyperthyroid phase of the post-partum thyroiditis that we are going to discuss soon.
It is very important to distinguish the clear difference between these two conditions, as they are caused by different factors and require different treatments. As mentioned earlier, hyperthyroidism, despite the increased appetite, causes weight loss to develop.
Weight loss can be dangerous during pregnancy and the breastfeeding period, as it is important for the mother to satisfy her daily requirements of the various nutrients, vitamins, and minerals.
Pregnant and breastfeeding mothers with hyperthyroidism, are exposed to the risks of premature delivery, low birth weight, and increased mortality for the mother and the baby.
The biggest impact of hyperthyroidism during breastfeeding is considered to be the interference with the milk let-down reflux due to the high thyroid hormone levels.
In normal circumstances, due to the let-down reflux, the milk is appropriately passed to the breastfeeding child. It has been reported that nursing mothers who have underlying hyperthyroidism are dealing with difficulties with their let-down reflux, as they are not able to feed their children propriety.
This will prevent the child from growing and developing as expected, as it will not be able to achieve and maintain the needed weight gain. [vi]
Post-partum thyroiditis
Post-partum thyroiditis, as the term suggests, is a condition that characterizes itself with an inflammation of the thyroid gland that has occurred in the first year after giving birth.
Post-partum thyroiditis has been reported in 5-7% of pregnancies worldwide.[vii] Post-partum thyroiditis can develop from either hyper or hypothyroidism.
Most of the symptoms are mild, which makes the process of diagnosing the issue a lot more difficult. Treatment of post-partum thyroiditis is planned according to which phase it is in.
Post-partum thyroiditis is known to cause the previously mentioned issues that have been linked to hypo- or hyperthyroidism. Most of the issues revolve around not having a good milk supply that your little one can use to grow and develop as expected.
Thyroid cancer
Thyroid cancer is the most serious issue of them all.
Early stages of thyroid cancer cause no visible symptoms, while symptoms such as difficulty swallowing, coughing, hoarseness, and pain in the neck and throat develop as cancer progresses. The most common treatment for thyroid cancer is surgery.
Thyroid cancer represents a major health issue for both the infant and the mother. Since it causes issues with the thyroid function, but most importantly, it requires radioactive therapy, chemotherapy, and radioactive iodine to be used during the treatment, breastfeeding during this period is not recommended.
Breastfeeding while taking thyroid medications
Each and every one of the thyroid issues that we have discussed today requires immediate treatment.
Any potential symptom should be reported to your doctor as soon as possible since underlying thyroid issues pose a great risk to our health.
Refusing and avoiding following a treatment plan for these issues is not recommended. By doing so, you are only putting yours and your baby’s life at risk.
The medications that are being used to treat hypothyroidism, with a focus on using levothyroxine, are considered to be safe to be used during pregnancy and breastfeeding. They work just like the normal thyroid hormones that are produced in your body.
The same goes for hyperthyroidism and the medications that are being used to treat this specific condition. Research suggests that nursing mothers nor infants are exposed to any risk by taking anti-thyroid medications to control their high thyroid hormone levels. [viii]
However, the use of radioactive iodine is not recommended to be used during pregnancy and breastfeeding.
If you have any concerns about following your treatment plan to treat your thyroid issues, do remind yourself about all the potential dangers that you and your baby can be exposed to if these thyroid issues are left untreated. Always remember to follow the advice and protocols of your doctor.
Conclusion
If you are experiencing problems trying to breastfeed your baby, it is possible that your thyroid is acting up.
This article discussed the many ways in which thyroid issues can impact breastfeeding. In short, there can be significant issues that can arise.
Be sure to consult your doctor and follow their advice regarding all procedures during and after pregnancy.
References
[i] Stuebe, A., MD, MSc. (2009). The Risks of Not Breastfeeding for Mothers and Infants. Reviews in Obstetrics and Gynecology,2(4), 222-231.
Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2812877/
[ii] Cataldo, N. A., Cooper, D. S., Chin, W. W., Maloof, F., & Ridgway, E. (1982). The effect of thyroid hormones on prolactin secretion by cultured bovine pituitary cells. Metabolism,31(6), 589-594. doi:10.1016/0026-0495(82)90097-x
Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/6804754
[iii] Stubert, J., Reister, F., Hartmann, S., & Janni, W. (2018). The risks associated with obesity in pregnancy. Deutsches Aerzteblatt Online. doi:10.3238/arztebl.2018.0276
Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5954173/
[iv] Galofré, J. C., Haber, R. S., Mitchell, A. A., Pessah, R., & Davies, T. F. (2010). Increased Postpartum Thyroxine Replacement in Hashimoto's Thyroiditis. Thyroid,20(8), 901-908. doi:10.1089/thy.2009.0391
Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2941405/
[v] Hage, M. P., & Azar, S. T. (2012). The Link between Thyroid Function and Depression. Journal of Thyroid Research,2012, 1-8. doi:10.1155/2012/590648
Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3246784/#sec11title
[vi] Breastfeeding and thyroid disease. (2017, August 01)
Retrieved from https://www.breastfeeding.asn.au/bfinfo/breastfeeding-and-thyroid-disease
[vii] Amino, N., & Kubota, S. (2011). Thyroid disease after pregnancy: Postpartum thyroiditis. Oxford Textbook of Endocrinology and Diabetes,552-557. doi:10.1093/med/9780199235292.003.3264
Retrieved from http://oxfordmedicine.com/view/10.1093/med/9780199235292.001.1/med-9780199235292-chapter-346
[viii] Hudzik, B., & Zubelewicz-Szkodzinska, B. (2016). Antithyroid drugs during breastfeeding. Clinical Endocrinology,85(6), 827-830. doi:10.1111/cen.13176
Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/27561657
























































Leave a comment