Thyroid and Blood Sugar Relationship
Both controlled by the endocrine system, the thyroid gland and your blood sugar levels (controlled by the pancreas) go hand in hand.
As such, a problem with one can lead to a problem with the other.
If you are suffering from a thyroid problem – or diabetes – then read on to learn more about the relationship between your thyroid and your blood sugar – and how it can affect your health in the long run.
The Endocrine System
The endocrine system is a group of cells and glands that produce hormones, molecules that regulate the activities of various organs and tissues in the body.
Included in this system is the thyroid gland, pituitary gland, adrenal gland, pancreas, testicles, and ovaries.
However, only those that will be discussed in detail are the glands relevant to this topic.
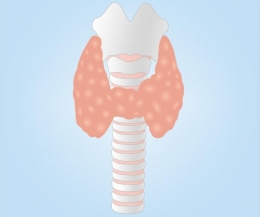
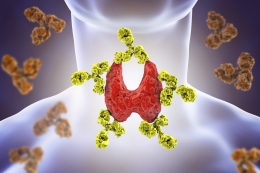
The Thyroid Gland
Located at the front of your neck, the thyroid gland is proof that great things come in small packages.
Shaped like a butterfly, this gland controls many vital functions in the body, such as your respiration, heart rate, body temperature, and digestion.
If your thyroid is inactive, it is not able to make the hormones that the body needs.
This condition is called hypothyroidism.
Symptoms include weight gain, cold intolerance, lower heart rate, fatigue, and muscle pain, to name a few.
On the other hand, if your thyroid is too active, it will produce more hormones than the body requires.
This condition, called hyperthyroidism, is characterized by heat intolerance, sleeping problems, mood swings, weight loss, and faster heart rate, among many others.
Pancreas
Located behind the stomach’s lower part is the pancreas, a gland responsible for making digestive enzymes as well as insulin, a hormone which regulates the body’s blood sugar levels.
Insulin is produced in the islets of Langerhans, alongside glucagon and other important hormones.
Blood Sugar Regulation
When you eat, glucose levels in the blood stream increase. This is regulated by different systems in the body, including the nervous system, gastrointestinal tract, liver, kidney, fats, and muscles.
Central to glucose regulation is the hormone insulin, which is produced by the beta-cells in the islets of Langerhans.
Insulin lowers blood sugar levels through the following mechanisms:
· Transport of glucose to the cells of the body, where it is converted as energy
· Conversion of glucose to glycogen (Glycogenesis) in the liver and muscles
· Formation of fat (Lipogenesis)
In the event that blood sugar levels dip below normal levels, the pancreas releases glucagon, which combats the effects of insulin.
As a result, sugar stores in the liver are released. Protein stores, on the other hand, are converted into sugar that will serve as the body’s source of energy.
Diabetes Mellitus
If blood sugar levels are not managed by the body properly, it can lead to the development of Diabetes Mellitus.
Also known as DM, it is a condition hallmarked by hyperglycemia or high blood sugar levels.
According to a study by Triplitt, predisposing factors include genetic/ environmental factors, age, lack of physical activity, obesity, fat accumulation in the torso area (central adiposity), and other pre-existing conditions.
DM is usually caused by a deficiency in insulin secretion or resistance to insulin action.
In the cases of increased insulin secretion, such as pregnancy, obesity, and excess cortisol, the pancreas compensates with increasing glucose levels in the body.
However, when insulin secretion is impaired, as in the case of beta-cell function loss, hyperglycemia takes place.
The problem is then worsened with insulin resistance, where glucose utilization in the tissues and muscles is lessened.
There are two types of DM:
· Type 1 DM is characterized by the inability of the body to make insulin. This is usually caused by the immune system destroying the beta-cells that synthesize insulin. Common in children and young adults, type 1 DM require insulin treatment for the rest of their lives.
· Type 2 DM, otherwise known as adult-onset diabetes, is a condition wherein the body does not make enough insulin, or is unable to utilize the insulin that it has. It develops over time, and is usually undiagnosed for several years.
Signs and symptoms of DM include:
o Increased thirst
o Frequent urination
o Tingling or decreased sensation in the hands and feet
o Infections with delayed healing
o Blurry vision
o Dry, itchy skin
o Unexplained weight loss
o Nausea and vomiting
o Irritability
o Tiredness and weakness
o Mood swings
Effects of Hypothyroidism on Blood Sugar Levels
Thyroid problems are present in 6.6% of the general population, with hypothyroidism accounting for most of the cases.
Unfortunately, this condition often coexists with type 1 and 2 DM. In fact, low thyroid function, as is the case in hypothyroidism, was pegged by Chaker et al as a risk factor in the development of DM, especially in people suffering from pre-diabetes.
In a 2014 study, Kalra stated that hypothyroidism leads to the development of hypoglycemia due to the numerous abnormalities that come with the former. These include:
· Low cortisol and growth hormone responses which prolong recovery from hypoglycemia
· Impairment in the processes of gluconeogenesis, or the creation of glucose, and glycogenolysis, or the breakdown of glycogen to glucose.
· Adrenal insufficiency which worsens hypoglycemia
· Reduced glucagon secretion and impaired glucagon effect on hepatocytes, resulting in slower insulin clearance
· Slow gastric emptying which delays glucose absorption in the intestines
Effects of Hyperthyroidism on Blood Sugar Levels
Hyperthyroidism is the polar opposite of hypothyroidism – as such, its effects on blood sugar is reversed as well.
In this thyroid disorder, hyperglycemia or high blood sugar develops, as stated in the study of Hage et al. This condition occurs because of the following mechanisms:
· Reduction of insulin half-life, due to degradation and release of insulin precursors
· Increase in the levels of proinsulin, or the building block of insulin
· Defective proinsulin processing as evidenced by a reduction in the C-peptide to proinsulin ratio
· Increase in glucose absorption due to increased levels of thyroid hormones
· Increase in GLUT2 levels which result to faulty glucose metabolism
· Increase in FFA that leads to fat breakdown (lipolysis) and the creation of glucose from non-carbohydrate substrates (gluconeogenesis)
· Overproduction of lactate that also enhances gluconeogenesis
Because of these, diabetics with hyperthyroidism often fail to control their sugar levels. In effect, long-term or chronic hyperglycemia can lead to many complications, including sexual dysfunction, foot ulcers, cardiovascular, and cerebrovascular diseases.
Similarly, thyrotoxicosis or excessive thyroid hormone in the body oftentimes leads to the development of diabetic ketoacidosis, or an increase in ketone levels due to body’s failure to produce the insulin that it needs.
Further Complications
The interrelatedness of thyroid problems and blood sugar regulation could not be refuted, but there is more to this than meets the eye.
For one, there is the development insulin resistance, which is characterized by the body’s inability to respond to insulin.
The beta-cells keep on producing insulin to meet the heightened demand, however, they eventually fail to meet the body’s needs. As a result, glucose builds up in the body, and this leads to prediabetes or type 2 DM.
Unfortunately, this condition has been shown to cause proliferative changes in the thyroid gland, as established in the study of Rezzonico et al.
Insulin resistance leads to thyroid tissue enlargement and the development of nodules that can progress into cancer.
Because of this, it has actually been identified as a risk factor in the development of differentiated thyroid cancer, as well as in other non-thyroid malignancies.
Vision problems fare higher in diabetic patients with hypothyroidism, compared to euthyroid individuals.
Studies even show that the development of nephropathy is increased in patients with subclinical hypothyroidism, as these people experience an increase in peripheral vascular resistance and a decrease in cardiac output.
These mechanisms lower the kidney’s filtration rate and blood flow, which then lead to kidney injuries.
What You Can Do
Both thyroid disorders and DM are lifetime conditions – meaning they are your burdens to bear for as long as you live.
Although this is the case, there are several things you can do in order to lower the risks of developing debilitating that come with the aforementioned illnesses.
Eat healthily
Being overweight is one of the many predisposing factors behind DM type 2.
The end goal of therapy is to manage your blood sugar levels, and you can do so by eating healthy meals and limiting your daily intake.
The National Institute of Diabetes and Digestive and Kidney Diseases recommends consuming smaller portions in order to cut back on your daily caloric intake. Trading healthier alternatives for fat-laden ones is another way to manage your DM.
Exercise!
Lack of physical activity is another risk factor that leads to the development of DM type 2.
Obesity promotes insulin resistance; it also increases one’s risk of developing thyroid cancer. However, decreasing your BMI can reduce this risk, according to a study by Aschebrook-Killfoy et al.
Other studies show that you can delay the development of the disease if you lose 5-7% of your current weight. In effect, exercising regularly – 30 minutes a day at 5 times a week – can help you curb the complications of both diabetes and its accompanying thyroid disorders.
Adhere to treatment regimens
Thyroid disorders are more prevalent in diabetics, compared to those without the disease. As such, this relationship plays a big role in the management of both diseases alongside each other.
With the glucose-lowering nature of hypothyroidism, patients are often prescribed lower doses of anti-diabetes medications. However, if your status is improving – as earmarked by a drop in thyroid-stimulating hormone (TSH) – the dosage of your anti-diabetes drugs will be increased.
As such, your thyroid status should be checked by the doctor from time to time so that he/she can determine the right dose of the medications.
Because of the interrelatedness of the two disorders, thyroid hormone replacement can help stabilize blood glucose levels in patients. It can also lead to better renal function as the effects of hypothyroidism has been linked with the eventual development kidney problems.
In individuals suffering from both thyroid and DM, treatment with Metformin has been proven effective in addressing both disorders.
Not only does it decrease insulin resistance and blood sugar levels in the body, another study by Kalra showed that it comes with a ‘thyroprotective’ effect. It means that the drug is able to reduce TSH levels in patients with hypothyroidism.
As a result, individuals taking this drug have a lower risk of developing thyroid cancer.
· Have regular check-ups
Consult with your doctor and undergo lab exams as warranted. As of late, research shows that some anti-diabetic agents can increase one’s risk of developing thyroid cancer.
Another study showed that those treated with the insulin analog Glargine posed a higher risk of developing thyroid cancer compared to those taking Human Insulin. As such, frequent clinic visits can help your physician assess which are the right medications for your preexisting conditions.
The relationship between thyroid disorders and DM – albeit bad – cannot be denied. As such, it is essential that you do everything in your power to maintain a healthy thyroid and normal blood sugar levels.
References:
Aschebrook-Kilfoy, B., Sabra, M. M., Brenner, A., Moore, S. C., Ron, E., Schatzkin, A., … Ward, M. H. (2011). Diabetes and Thyroid Cancer Risk in the National Institutes of Health-AARP Diet and Health Study. Thyroid, 21(9), 957–963. http://doi.org/10.1089/thy.2010.0396
Chaker, L., Ligthart, S., Korevaar, T. I. M., Hofman, A., Franco, O. H., Peeters, R. P., & Dehghan, A. (2016). Thyroid function and risk of type 2 diabetes: a population-based prospective cohort study. BMC Medicine, 14, 150. http://doi.org/10.1186/s12916-016-0693-4
Hage, M., Zantout, M., & Azar, S. (2011). Thyroid Disorders and Diabetes Mellitus. Journal of Thyroid Research. Retrieved August 24, 2017, from https://www.hindawi.com/journals/jtr/2011/439463/.
How does the pancreas work? (2016, December 30). Retrieved August 25, 2017, from https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072490/
Kalra, S., Dhamija, P., & Das, A. K. (2012). Metformin: Midlife maturity, maiden charm. Indian Journal of Endocrinology and Metabolism, 16(6), 1015–1018. http://doi.org/10.4103/2230-8210.103028
Kalra, S., Unnikrishnan, A. G., & Sahay, R. (2014). The hypoglycemic side of hypothyroidism. Indian Journal of Endocrinology and Metabolism, 18(1), 1–3. http://doi.org/10.4103/2230-8210.126517
Prediabetes & Insulin Resistance. (2009, August). Retrieved August 24, 2017, from https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance
Rezzonico, J., Rezzonico, M., Pusiol, E., Pitoia, F., & Niepomniszcze, H. (2008). Introducing the thyroid gland as another victim of the insulin resistance syndrome. [Abstract]. Thyroid,18(4), 461-464. Retrieved August 24, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/18346005?dopt=AbstractPlus.
Triplitt, C. (2012). American Journal of Managed Care, 18, 4-10. Retrieved August 24, 2017, from http://www.ajmc.com/journals/supplement/2012/ace005_12jan_glucose/ace005_12jan_triplitt_s4/P-3
Type 1 Diabetes. (2017). Retrieved August 24, 2017, from http://healthcare.utah.edu/utahdiabetescenter/type-1.php
Type 2 Diabetes. (2017). Retrieved August 24, 2017, from http://healthcare.utah.edu/utahdiabetescenter/type-2.php
























































Leave a comment