Thyroid and Headaches
Thyroid and Headaches Relationship
Do you suffer from headaches every so often?
While it can be due to tension or stress, there is another underlying pathology that should be considered: thyroid disorder.
Though seemingly unrelated, recent researches show that headaches and thyroid dysfunctions might be actually be linked to one another.
What are Headaches?
A headache is one of the most common forms of pain.
It is experienced by 2 out of 3 children before they reach age 15, with 9 out of 10 adults suffering from severe headaches at one point in their lives. It is a pivotal reason behind people missing out on school or work.
As such, it is a major driving force behind most individuals’ visits to the doctor.
Frequency and severity of headaches vary from person to person.
While the brain itself cannot feel pain due to its lack of pain-sensitive nerves, headaches occur when nociceptors or pain-sensitive nerve endings react to factors that cause headaches (examples include medications, stress, or odors, to name a few.)
Messages are then sent from the trigeminal nerve to the thalamus, which relays the ‘pain sensation’ to the different parts of the body.
There are several types of headaches:
Primary Headaches
This headache occurs independently and is not activated by any medical condition. What causes primary headaches are still a mystery to experts.
However, some posit that events that affect the blood vessels and nerves bring about signals to the brain – this is then the pain experienced as a headache.
Examples of primary headaches include cluster headaches, tension headaches, and migraines.
Cluster Headaches
Tagged as the most severe form of primary headaches, cluster headaches are characterized as sudden and intensely painful.
Such headaches occur in “clusters,” usually at the same time of the day for a few weeks. It usually affects one side of the head, around or behind an eye, with the affected side getting swollen and reddened.
This headache occurs more in men than women, with the symptoms starting at age 20 and lasting up to age 50. Frequency is often at 1 to 3 cluster headaches a day.
It is considered seasonal, as it occurs more often in spring and autumn. As such, it is mistaken as allergic symptoms, which is why cluster headaches are usually hard to diagnose and treat.
Tension-type Headaches
Previously known as muscle contraction headaches, this commonly-occurring condition is influenced by stress, as well as emotional and mental conflicts. Tension-type headaches affect more women than men.
The pain is characterized as mild to moderate, and felt on both sides of the head. The pain subsides usually once the cause is eliminated.
One form of tension-type headache is the episodic type, which can occur 10 to 15 times a month. The attack can last anywhere from 30 minutes to several days.
The chronic type, on the other hand, occurs more than 15 days a month in a three-month period.
Migraines
Migraines affect approximately 12% of the American people, with women affected three times more than men. Family history and other medical conditions can also influence one’s migraine attacks.
Migraine occurs due to the activation of nerve fibers near various brain blood vessels. The pain is characterized as pulsating and throbbing, often affecting one side of the head.
It often occurs in the morning upon waking up, though times can vary. Triggers vary from weather changes to intake of chocolate or aged cheeses. Hormonal changes in women can affect migraine episodes as well.
Migraines can be accompanied by light, noise, or odor sensitivity, as well as nausea and vomiting. If left untreated, the migraine episode can last anywhere from 4 to 72 hours. The pain can be worsened with coughing, sneezing, movement, and routine physical activity.
Like headaches, there are different types of migraines. The major types are the following:
- Migraine with aura. Previously known as classic migraines, this comes with visual disturbances and neurological symptoms (speaking troubles, muscle weakness, numbness, etc.) that occur 10-60 minutes before the actual migraine. The duration is limited to an hour tops.
- Migraine without aura. Known as the more frequent form or the common migraine, it comes with headache pain that happens without warning. It occurs on one side of the head, and often comes with confusion, nausea, blurred vision, fatigue, and mood changes, to name a few.
Secondary Headaches
Secondary headaches, on the other hand, are symptoms of another health condition. It occurs when nerve endings (which are pain-sensitive) are displaced.
This can be caused by head injury, tumors, stroke, infection, fever, medication overuse, high blood pressure, emotional conflict, and stress, to name a few.
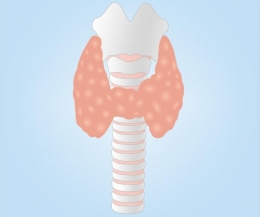
The Interconnectivity of Thyroid Disorders and Headaches
Headaches are indeed associated with hypothyroidism, as concluded in many researches. One to do so is the study of Martin et al.
This longitudinal retrospective cohort study observed patients who complained of headaches, and were not diagnosed by thyroid disease previously.
The study ran for 20 years, and results showed that in the 26% of the population who were confirmed to have headache disorders, more or less than 7% developed hypothyroidism.
Numerically, this places the hazard ratio for the development of hypothyroidism at 1.21 for patients suffering from headache disorders.
More than just headaches, migraines have been associated with thyroid disease as well. A study conducted by experts from the University of Cincinnati College of Medicine (UCCM) showed that individuals suffering from headaches and migraine are at a greater risk of developing hypothyroidism.
Results show that those who suffer from cluster headaches have a 21% risk of developing hypothyroidism, while those with migraine have a staggering 41% chance of developing hypothyroidism. Although this is the case, experts are unclear as to how the two conditions are interconnected.
It was also determined that apart from overt hypothyroidism, subclinical hypothyroidism is also associated with migraine. Subclinical hypothyroidism is a mild, early form of hypothyroidism. In this condition, TSH levels are above normal, while thyroid gland hormones are within the normal range.
As per the case-control study of Rubino et al, 151 subclinical hypothyroidism patients were matched with 150 controls. Migraine characteristics and parameters were obtained from both groups and were compared accordingly.
Results showed that those with subclinical hypothyroidism had a 46% prevalence of developing lifetime migraine, compared to the control group’s 13%. Migraine with or without aura was higher in hypothyroid patients as well.
Further studies suggest that most hypothyroid patients have experienced migraine episodes as children. In fact, some experts say that thyroid disease could be a risk factor in the progression of episodic migraine to chronic migraine.
Even with many studies supporting the interconnectivity of headaches and hypothyroidism, even experts are baffled as to why the two go hand-in-hand together. There are many theories though, as stated by UCCM study author Dr. Vincent Martin.
For one, it could be the result of an overactive immune system, with the frequent headaches making the body more vulnerable to thyroid disease. Other factors considered are inflammation, environment, genetic factors, even the medications taken to treat headaches.
Headache Manifestations in Thyroid Disorders
A study by Carvalho et al delved into the prevalence, characteristics, and treatment of headaches associated with recent onset hypothyroidism.
Results showed that at least 34% of the subjects complained of headaches, with majority of them localizing the event in the fronto-parietal region. 37% suffered from temporally-located headaches, while 15% pinpointed the location to the back of their heads.
As for the features, 63% described their headaches as pulsatile, while 78% verbalized that they lasted anywhere from 4 to 72 hours.
Most described their headaches as something moderate to severe in intensity, while 60% complained that it came with nausea and vomiting. 47% of the respondents, on the other hand, described the headache as unilateral in location.
The complaints of the subjects shed light into the fact that headaches associated with thyroid disorders vary in characteristic and prevalence.
Some people characterize such headaches as constant and non-throbbing, affecting both sides of the head. For some, they do not come with nausea or vomiting, which make them seem like tension headaches more than migraine headaches.
However different the symptoms might be, experts agree on one thing: the severity is proportional with severity of the disease. This means if that the hypothyroidism symptoms worsen, it is expected that the headaches symptoms will aggravate as well.
This is supported by the statement of Dr. Vincent Martin, co-author of the UCCM paper: "It is possible that the development of hypothyroidism in a headache patient might further increase the frequency of headache, as past studies have found that treatment of hypothyroidism reduces the frequency of headache.”
With that being said, Martin advises physicians to consider checking for hypothyroidism in patients suffering from frequent headache episodes.
Thyroid Treatment Relieves Headaches
Since hypothyroidism and headaches are connected, experts recommend patient adherence to thyroid disease treatment in order to reduce headache severity.
Such was proven in the study by Carvalho et al, where Levothyroxine treatment brought about a decrease in the incidence of hypothyroidism symptoms, especially its associated headaches.
Not only does this apply to adults, the same findings were seen in the study of children as well. The research of Mirouliaei et al delved with the efficacy of Levothyroxine in migraine headaches in children suffering from subclinical hypothyroidism.
This follows the central thought of many associated papers: that hypothyroidism could be an exacerbating factor in the development of primary headaches and migraines, whether in adults or children.
The quasi-experimental study features 25 migraineur children who were diagnosed with subclinical hypothyroidism. After evaluation, these participants were treated with Levothyroxine.
True enough, the subjects noted lesser frequencies of headaches (from a max of 17 times a month to just once a month.) Severity of the headaches reduced as well from a max score of 6.24 to just 0.87.
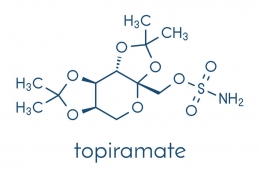
Levothyroxine
As seen in the studies above, Levothyroxine treatment is deemed as the saving grace not only for hypothyroidism – but for the associated headaches as well.
This thyroid hormone works by replacing the lacking thyroid hormone in the body. Such is the case in hypothyroidism, where the thyroid gland is unable to synthesize the needed amounts of thyroid hormone in the body.
Without adequate amounts of thyroid hormone, hypothyroidism symptoms can occur. These include fatigue, hair loss, weight gain, constipation, joint and muscle pain, depression, and thick skin, to name a few.
Levothyroxine’s common brand names include Levo-T, Levothyroid, Synthroid, Levoxyl, Tirosint, and Unithroid. It comes in tablet and capsule forms, and is usually taken once a day before meals. The dosage can range from 50 to 100 micrograms, depending on the doctor’s assessment.
While Levothyroxine treatment works right away, it might take weeks for you to notice changes in symptoms. This does not mean that you should increase your dosage, as doing so can bring about unpleasant side effects, which might include diarrhea, vomiting, muscle cramps, shaking, restlessness, and excitability.
References:
Carvalho, M. L., De Medeiros, J. S., & Valenca, M. M. (2017). Headache in recent onset hypothyroidism: Prevalence, characteristics and outcome after treatment with levothyroxine [Abstract]. Cephalalgia,37(10). doi:10.1177/0333102416658714
Headache: Hope Through Research. (2018, July 6). Retrieved September 25, 2018, from https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Hope-Through-Research/Headache-Hope-Through-Research
Levothyroxine: MedlinePlus Drug Information. (n.d.). Retrieved September 25, 2018, from https://medlineplus.gov/druginfo/meds/a682461.html
Macmillan, A. (2016, September 30). If You Get Frequent Headaches, You May Want to Have Your Thyroid Tested. Retrieved September 25, 2018, from https://www.health.com/thyroid/hypothyroid-headaches-migraines
Martin, A. T., Pinney, S. M., Xie, C., Herrick, R. L., Bai, Y., Buckholz, J., & Martin, V. T. (2016). Headache Disorders May Be a Risk Factor for the Development of New Onset Hypothyroidism. Headache: The Journal of Head and Face Pain,57(1), 21-30. doi:10.1111/head.12943
MIROULIAEI, M., FALLAH, R., BASHARDOOST, N., PARTOVEE, M., & ORDOOEI, M. (2012). Efficacy of Levothyroxine in Migraine Headaches in Children with Subclinical Hypothyroidism. Iranian Journal of Child Neurology, 6(4), 23–26.
Rubino, E., Rainero, I., & Garino, F. (2018). Subclinical hypothyroidism is associated with migraine: A case-control study. Cephalalgia. doi:10.1177/033310241876991
Preidt, R. (2016, September 29). Can You Blame Your Headaches on Your Thyroid? Retrieved September 21, 2018, from https://www.webmd.com/migraines-headaches/news/20160929/can-you-blame-your-headaches-on-your-thyroid
























































Leave a comment